TREATMENT OF PEPTIC ULCER
Peptic ulcer was one of the most common gastric disease. After introducing drugs like proton pump inhibitors , antacids ,etc number of peptic ulcer cases have gone down drastically .
Before learning about the drugs for treatment of peptic ulcer one must have a thorough knowledge about the physiology of peptic ulcer formation.
Peptic ulcer occurs due to imbalance between DEFENSIVE FACTORS AND AGGRAVATING FACTORS
DEFENSIVE FACTORS
- MUCUS
- BICARBONATE
- MUCOSAL BLOOD FLOW
AGGRAVATING FACTORS
- GASTRIC ACID
- NSAID'S
- CORTICOSTEOIDS
- HELICOBACTER PYLORI
- ALCOHOL
- SMOKING
Due to the imbalance, patient initially suffers through gastritis ie. inflammation of gastric mucosa due to gastric irritation by aggravating factors (alcohol,NSAID's,etc) .
If this gastritis persists it will lead to peptic ulcer .
This can be acute or chronic
Next we will see about gastric acid synthesis and regulation which is very important to understand the mechanism of action of drugs .
Parietal cell is responsible for secretion of gastric acid.
Parietal cell is stimulated by number of factors :
- When a person thinks about food , gastric acid gets secreted . it is because of stimulation in brain which transmits impulses via vagus nerve which in turn stimulates the M 1 receptor on the Enteric nervous system (ENS) . ENS will secrete Ach which will act on M 3 receptor of gastric mucosa . (REFER ABOVE DIAGRAM)
- When food reaches the stomach G CELL gets stimulated . G cell produce gastrin , which will act on CCK-B receptor on parietal cell . thus secreting gastric acid .(DIAGRAM)
- Histamines are released from Entero chromatoffin like cell -2 present in the sub mucosa . Released histamine will act on H2 receptor of parietal cell. ECL -2 secretes histamine throughout the day thus responsible for basal gastric acid secretion .(DIAGRAM)
Thus we saw about the physiology of gastric acid secretion . Next we will move on to the treatment of peptic ulcer .
DRUGS USED IN PEPTIC ULCER
- ANTACIDS
- PROTON PUMP INHIBITORS
- H2 RECEPTOR ANTAGONISTS
- ANTICHOLINERGICS M 1 BLOCKERS
- DRUGS INCREASING PROTECTIVE FACTORS
- ULCER PROTECTIVE DRUGS
- ULCER HEALING DRUGS
- ANTI HELICOBACTER DRUGS
1)ANTACIDS
MECHANISM OF ACTION : These drugs are weak bases , they neutralize the gastric acid .
DRUGS: Sodium bicarbonate , Aluminium hydroxide , magnesium hydroxide , MEGALDRATE , Magnesium tricilicate .
PHARMACOKINETICS:
- All antacids are taken orally
- Only Sodium bicarbonate is absorbed systemically .
- Sodium bicarbonate is faster acting but has short period of action
- Other antacids are not absorbed .
- Other antacids have slower onset of action but have longer period of action
USE:
- They give prompt pain relief in Peptic ulcer
- Treatment for Hypophosphatemia.
ADVERSE EFFECTS:
- Sodium bicarbonate uses bleching and gastric distention due to the release of CO2
- Aluminium hydroxide causes constipation
- Magnesium hydroxide causes diarrhoea .
THUS combination of magnesium and aluminium hydroxide is used . It is called as MEGALDRATE .
2)PROTON PUMP INHIBITORS
MECHANISM : These drugs by irreversibly inhibiting H+K+ATPase in parietal cells . Thus meal stimulated and basal acid output is decreased .
DRUGS : Omeprazole , Pantoprazole , Lansoprazole , Rabeprazole
PHARMACOKINETICS :
- These drugs taken orally and I.V
- These are PRODRUGS.
- They are converted to active form SULFENAMIDE (not sulphonamide which is an antibiotic. ) in Parietal cells .
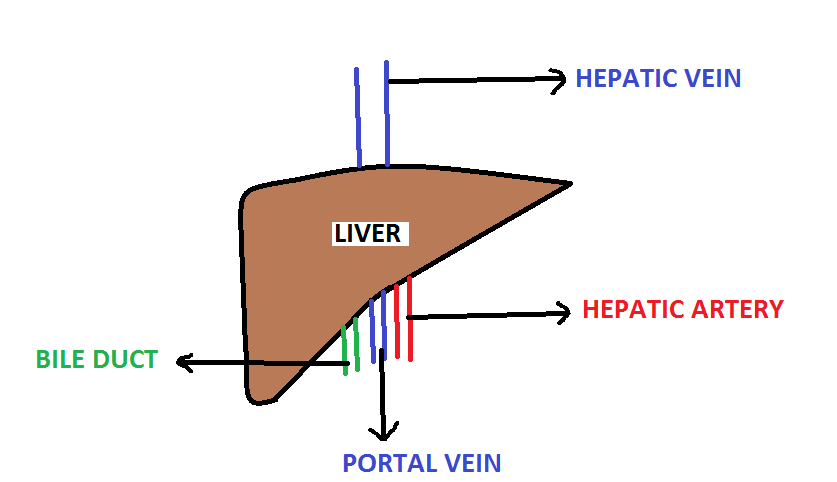
- They are metabolized in liver
- They are excreted in Urine
USE :
- Peptic ulcer
- GERD
- Zollinger-Ellison diesease
- Lansoprazole is given in pregnancy
ADVERSE EFFECTS :
- Decrease Vit-B 12 absorption
- Decrease Ca absorption
- Decrease iron absorption
- Diarrhoea
3)H2 RECEPTOR ANTAGONIST :
MECHANISM: These drugs competitively inhibit H2 receptor in parietal cell , thus inhibits gastric acid secretion
Ach and Gastrin also acts partially by releasing histamine . Action of these agents are also decreased partially by these drugs .
DRUGS : Cimetidine , Ranitidine , Famotidine , Roxatidine
PHARMACOKINETICS :
- Taken orally
- Systemic absorption of the drug happens
- They are excreted unchanged in urine
- It crosses placenta
- Potency and Longer action ---- Cimetidine < Ranitidine < Famotidine < Roxatidine
USES:
- Peptic ulcer diesease
- Drug of choice for stress induced ulcer
- GERD
- Zollinger-Ellison Syndrome
- Prophylaxis of aspiration pneumonia
ADVERSE EFFECTS :
- Headache
- Diarrhoea
- Cimetidine has anti-androgenic effect
- Cimetidine is an enzyme inducer
ANTICHOLINERGIC DRUGS:
PIRENZEPINE AND TELENZEPINE are selective M1 blockers .
Thus used in peptic ulcer disease .
DRUGS INCREASING PROTECTIVE FACTORS :
Prostaglandin E and Prostaglandin I2 play an important role in secretion of protective factors and inhibition of gastric acid secretion .
Thus Prostaglandin analogue can be given in peptic ulcer disease .
Prostaglandin E analogue called Misoprostol is the commoly used drug .
ULCER PROTECTIVE AGENTS :
MECHANISM: These drugs form a coating over the gastric mucosa and thus protect from the exposure of acid .
DRUGS:
- SUCRALFATE
- COLLOIDAL BISMUTH SUBCITRATE
These drugs should not be given with antacids because these drugs are active only in acidic medium . Antacids creates a basic pH in stomach .
ULCER HEALING DRUGS :
CARBENOXOLONE is the drug for healing of ulcer .
ANTI HELICOBACTER PYLORI DRUGS :
Commonly used regimen for treatment of H.pylori is TRIPLE DRUG THERAPY .
TRIPLE DRUG THERAPY is
PROTON PUMP INHIBITOR (Lanoprazole 30mg or pantoprazole 40 mg ) + AMOXICILLIN 1000 mg + CLARYTHROMYCIN 500 mg twice daily for 2 weeks .
HERE ENDS THE TOPIC . IF ANYONE HAS DOUBTS OR HAS EXTRA POINTS TO ADD TO THIS BLOG PLEASE DO COMMENT.